|
Key Takeaways:
|
When you hear the phrase “menstrual cycle”, a lot of people associate it with the few painful days of cramps, exhaustion, and discomfort. But, your menstrual cycle is more than just your period, and shedding the lining of your uterus is just one phase in a four-phase cycle. It’s a rollercoaster ride of fluctuating hormones and changing symptoms that can take anywhere from 24 to 38 days to complete.1 2
What can you expect throughout this hormonal journey? Here’s a quick guide to your menstrual cycle, and what’s happening in your body in each phase.
What Is the Menstrual Cycle?
Your menstrual cycle starts on the first day of your period and ends on the first day of your next period. Between the two are a series of events that occur in your body as it prepares for the possibility of pregnancy.1
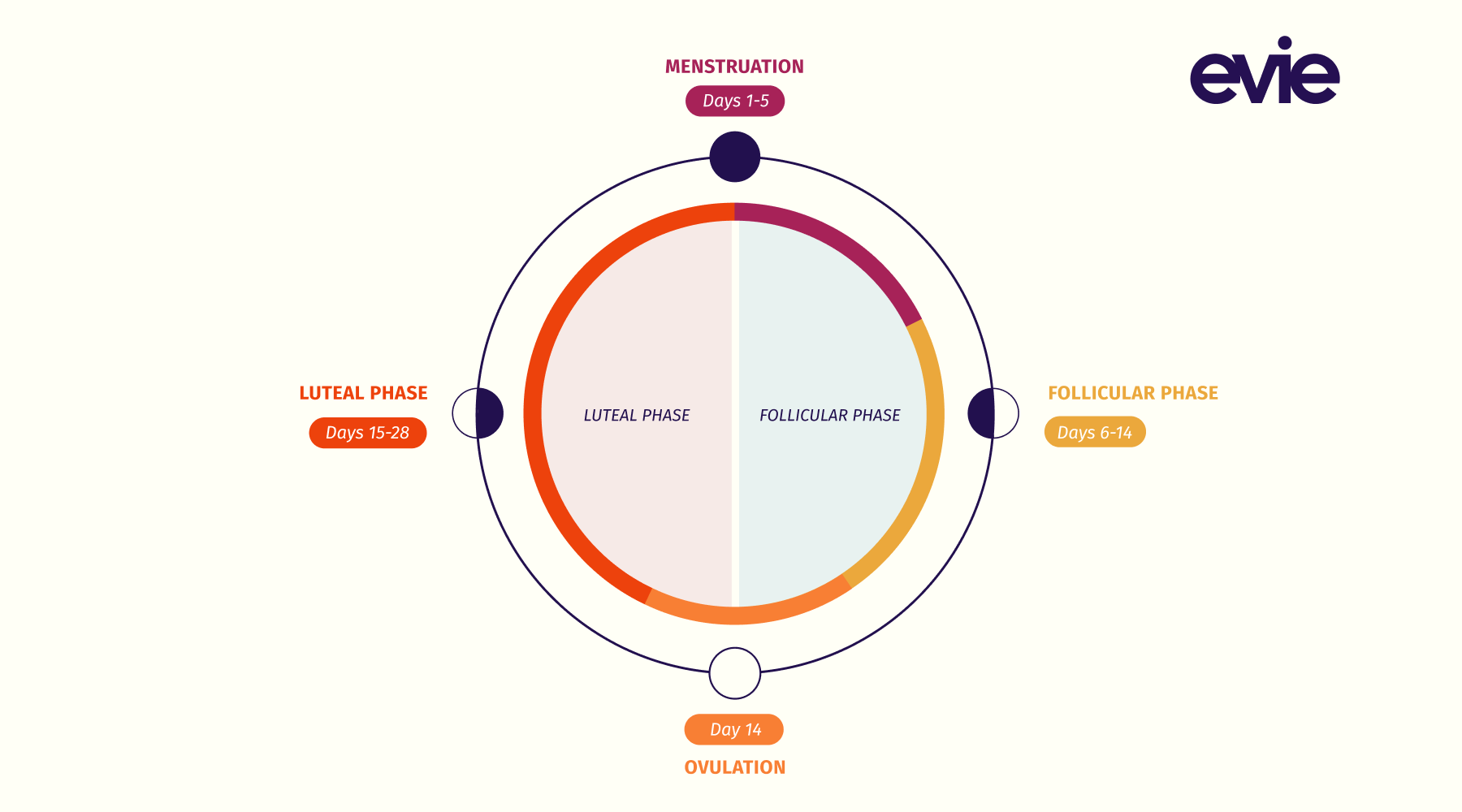
There are four phases to the menstrual cycle:1
- Menstruation
- Follicular phase
- Ovulation
- Luteal phase
Hormones drive each phase of this menstrual cycle. And these hormonal changes can have a wide array of effects on everything from your energy levels to sleeping habits to exercise performance. Although everyone who menstruates may experience these phases and hormone changes differently, the process is the same.1

The Menstrual Cycle Phases
Phase 1: Menstruation
Days 1-5
What’s happening with your hormones?
Progesterone and estrogen are at their lowest.
What’s going on in your body?
The most talked-about phase in the menstrual cycle also happens to be the most uncomfortable for many people: menstruation. This is when your body is shedding the lining of your uterus or endometrium.1 2
Before shedding, your body was increasing your estrogen and progesterone levels to help thicken the walls of your endometrium in preparation for a fetus.2 When fertilization doesn’t occur, your body discards those extra layers of your endometrium, along with blood and mucus, through the vagina.2
The first day of your period is day one of your menstrual cycle. It lasts anywhere from three days to a week and, for many, is often accompanied by painful or uncomfortable symptoms like cramps, headaches, fatigue, nausea, and more.3
Phase 2: Follicular Phase
Days 6-14
What’s happening with your hormones?
Estrogen levels start to rise, reaching their highest point in this phase. The brain also releases gonadotropin-releasing hormone (GnRH) and follicle-stimulating hormone (FSH).
What’s going on in your body?
Technically, menstruation is part of the follicular phase. But it’s separate because menstruation is only the beginning. The follicular phase starts on day one of your cycle and ends around day 14 when you begin ovulation.
At the start of this phase, your hormone levels are at their lowest. But as you progress from day one to day 14, your estrogen levels start to rise.4 The brain also releases several hormones including a gonadotropin-releasing hormone (GnRH) and follicle-stimulating hormone (FSH). These hormones trigger the production of follicles in each of your ovaries.5 6 Hence the name “follicular” phase.
There are thousands of follicles in the ovaries, and each contains an immature egg. From day 10 to day 14 of your menstrual cycle, around 11 to 20 eggs will complete maturation but only one will go through to ovulation.6 7 During this phase, your body also restarts the process of thickening the lining of your uterus in preparation for a possible pregnancy.1 5

Phase 3: Ovulation
Day 14
What’s happening with your hormones?
Estrogen levels drop from their highest point as progesterone begins its steady climb. And a spike in the luteinizing hormone (LH) triggers ovulation.
What’s going on in your body?
On average, ovulation takes place around day 14 in your cycle or around two weeks before your next period. During ovulation, an increase in the luteinizing hormone (LH) causes the release of a mature egg from the surface of the ovary.1 The egg then travels along your fallopian tube to your uterus.5 During this time you may experience spotting or discomfort in your abdomen, but some people don’t experience any symptoms.2
You have a fertilization window of around 24 hours as your egg makes this journey. This means your best chance of getting pregnant is during ovulation or up to three to five days before.5 This gives sperm the opportunity to fertilize the egg as it travels along the fallopian tube. But, if the egg doesn’t become fertilized, you’ll begin the process all over again.2
Phase 4: Luteal Phase
Days 15-28
What’s happening with your hormones?
Both estrogen and progesterone levels rise, with progesterone reaching its highest during this phase. But if there is no fertilization, both hormone levels will drop to repeat the cycle all over again.
What’s going on in your body?
The last phase of your menstrual cycle is the luteal phase. It starts after ovulation and ends when you begin your next period. This phase, which lasts around two weeks, is all about preparing your body for pregnancy (if fertilized) or your next period (if not fertilized).
After the follicle releases the egg during ovulation, it changes into a structure called the corpus luteum.8 The corpus luteum increases your progesterone and estrogen levels, causing the lining of your uterus to thicken so it’s easier for a fertilized egg to implant and grow. Progesterone reaches its highest during this phase.
But if you’re not pregnant, the corpus luteum dissolves and your hormone levels drop. This sends a signal to your brain that it’s time to repeat the menstrual cycle from the beginning as you start the first day of your period.
How Does Your Menstrual Cycle Change as You Age?
Most people begin their menstrual cycle around the age of 12, but you can start menstruating anywhere from 8 to 16 years old.1 In those first few years, it’s normal to experience a heavier or irregular flow. But as you age, your cycle tends to follow a more consistent schedule.1
However, fluctuations or changes in your cycle can occur throughout your life, especially during hormone-changing events like pregnancy or lactation.1 Changes to your cycle also occur as you make the transition to menopause, with many experiencing irregular periods or spotting. This transition period is called perimenopause, and it often begins in your late 30s or early 40s.9
Perimenopause can last anywhere from eight to ten years as your body slowly produces less and less estrogen. You’re still following your menstrual cycle and can get pregnant during this time. But after 12 consecutive months without a period, you’ve officially entered menopause. It’s at this point that your menstrual cycle stops and your ovaries no longer release eggs.9
The Takeaway
The menstrual cycle is a hormonal journey your body takes every 24 to 38 days to prepare for pregnancy. For most menstruating adults, this cycle begins around age 12 and ends with menopause in your late 40s or early 50s. It includes four phases: menstruation, follicular phase, ovulation, and the luteal phase.
Throughout each phase, you’re experiencing a rise and fall in hormones like estrogen and progesterone. Although all menstruating adults follow the same four phases of the menstrual cycle, that doesn’t mean we all experience our menstrual cycle the same. It’s a different journey for everyone with varying symptoms and experiences. And your menstrual cycle could also change over the years as you experience various life events or experiment with different methods of birth control.
Sources
- Menstrual Cycle (Normal Menstruation): Overview & Phases. (2022, December 9). Cleveland Clinic. Retrieved March 16, 2023, from https://my.clevelandclinic.org/health/articles/10132-menstrual-cycle
- Menstrual Cycle: An Overview. (2019, December 26). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/wellness-and-prevention/menstrual-cycle-an-overview
- Daley, A. (2008). Exercise and Primary Dysmenorrhoea. Sports Medicine, 38(8), 659–670. https://doi.org/10.2165/00007256-200838080-00004
- U.S. Department of Health and Human Services. (2021, February 16). Physical activity and your menstrual cycle. Office on Women’s Health. Retrieved March 16, 2023, from https://www.womenshealth.gov/getting-active/physical-activity-menstrual-cycle
- Department of Health & Human Services. (2022, June 9). Menstrual cycle. Better Health Channel. Retrieved March 16, 2023, from https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/menstrual-cycle
- Monis CN, Tetrokalashvili M. Menstrual Cycle Proliferative And Follicular Phase. 2022 Sep 12. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 31194386.
- Follicular Phase Of Menstrual Cycle: Hormone Levels & Length. (2022, August 8). Cleveland Clinic. Retrieved March 16, 2023, from https://my.clevelandclinic.org/health/body/23953-follicular-phase
- Luteal Phase Of The Menstrual Cycle: Symptoms & Length. (2022, November 4). Cleveland Clinic. Retrieved March 16, 2023, from https://my.clevelandclinic.org/health/articles/24417-luteal-phase
- Menopause: What It Is, Age, Stages, Signs & Side Effects. (2021, October 5). Cleveland Clinic. Retrieved March 30, 2023, from https://my.clevelandclinic.org/health/diseases/21841-menopause
- Phases of The Menstrual Cycle Explained. (2022, September 26). Elara Care. https://elara.care/hormones/video-phases-of-the-menstrual-cycle-explained/