|
Key Takeaways:
|
From waking up in a hot sweat to going to the bathroom more times than usual, it’s normal for menopause-like symptoms to start to reveal themselves as you end your 30s and enter your 40s. But you can’t be starting menopause yet…right?
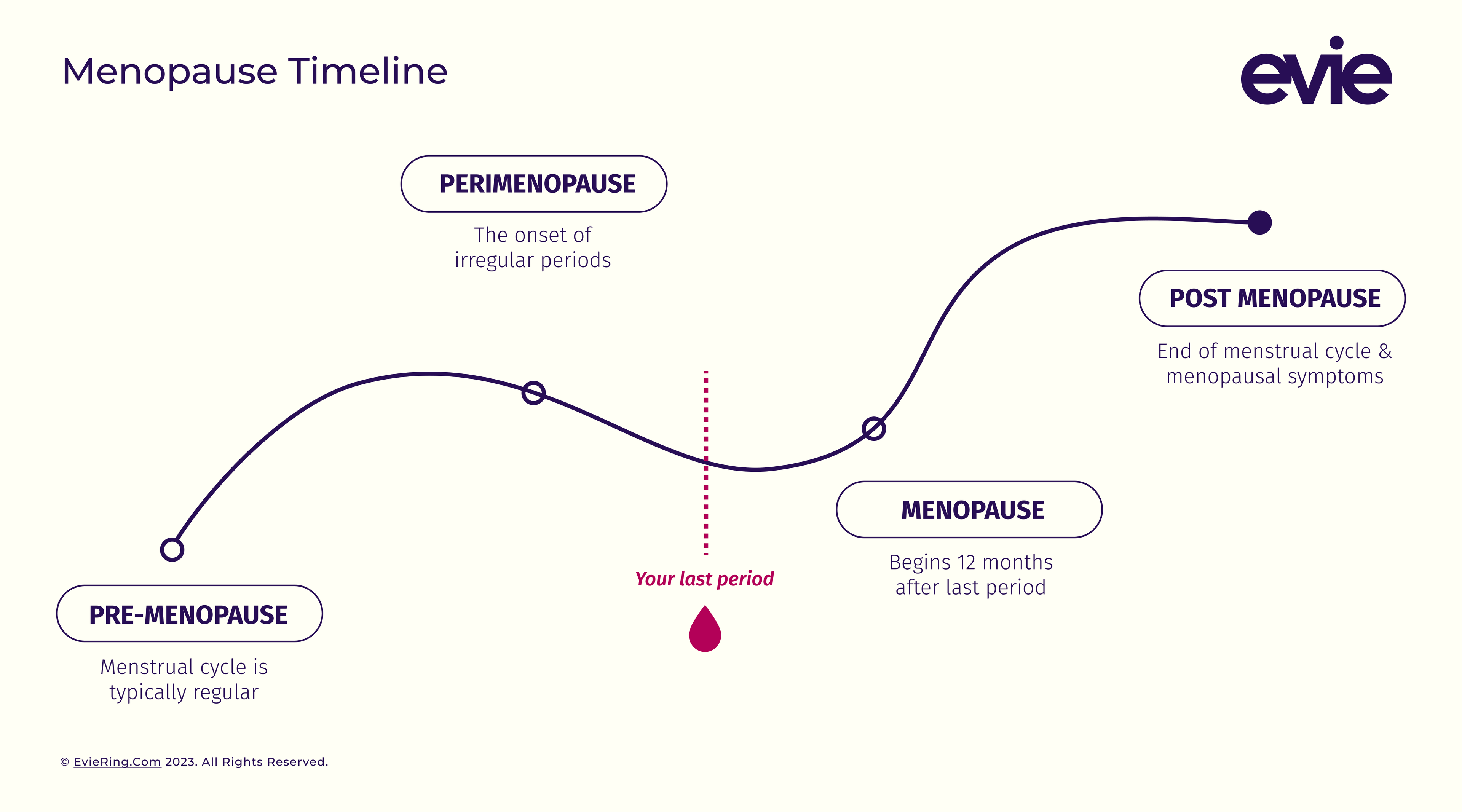
For most women, menopause starts in their 50s. But it doesn’t happen overnight. Before you enter menopause your body is going through several changes as you transition away from your reproductive years. And this period of your life is called perimenopause.
What Is Perimenopause?
Perimenopause is your body’s transition to menopause or the end of your menstrual cycle.1 This transition can last anywhere from 2 to 10 years.2 During this time, your body is still moving through the phases of your menstrual cycle — which means yes, you can still get pregnant. However, you’re producing fewer hormones like estrogen and your ovaries slowly stop releasing as many eggs.2 3
These hormonal changes often introduce irregular periods and early menopause symptoms like hot flashes, headaches, and vaginal dryness. As you get closer to menopause, you start having fewer and more infrequent periods. Then, after 12 months without a period, you’ve officially entered menopause.1 3
Perimenopause vs Menopause
Perimenopause is the transition to menopause while menopause signifies the end of your reproductive cycle.3 In other words, if perimenopause and menopause were stops on the train ride that is your reproductive journey, perimenopause would be the last few stations and menopause would mark the end of the reproductive line. They’re both natural and normal parts of aging. And although menopause marks the end of your fertility, it also marks the beginning of a new phase of your life.
When Does Perimenopause Start?
Throughout most of your reproductive life, your cycle should be fairly predictable. Your hormones rise and fall in constant preparation for pregnancy. But when that predictability starts to shift and you notice more irregularity in your cycle, this is a sign you’ve entered perimenopause.4 5
Most women enter perimenopause in their mid-40s. But some start perimenopause as late as their 50s or as early as their 30s. Some experience a short transition period to menopause. For others, the transition lasts a lot longer. But the commonality among those who enter perimenopause is that your period is no longer following its familiar schedule.3
How Long Does Perimenopause Last?
The age you enter perimenopause varies from person to person, as does the length of that transition. For most people, perimenopause starts in their 40s and lasts three to four years. It could also last as little as a few months or stretch out over a decade. It all depends on the person and factors like your medical or family history. When your ovaries stop producing eggs and your periods have ceased for over 12 months, perimenopause ends and menopause begins.4 5

Symptoms of Perimenopause
As you transition away from your reproductive years, you might notice other signs that you’re entering perimenopause, like hot flashes, difficulty sleeping, or increasing feelings of depression or anxiety. Many women experience physical and mental symptoms as a result of the hormonal changes going on in their bodies, especially in those last few years of perimenopause as your estrogen levels drop significantly.4
Although not everyone encounters these symptoms, the most common ones include:2 3 4
- Erratic, infrequent, or heavy periods
- Hot flashes
- Night sweats
- Heart palpitations
- Difficulty sleeping
- Irritability & mood swings
- Depression or anxiety
- Vaginal dryness
- Lower or changing sex drive
- Headaches
- Urinary changes (like needing to use the bathroom more often)
- Joint and muscle aches
- Breast tenderness
- Fatigue or exhaustion
- Difficulty concentrating
Your body has been producing estrogen since puberty. Think of these symptoms as your body’s way of adjusting to your new hormone levels.3 This adjustment period is temporary, and its intensity and duration vary from person to person. Even though these symptoms are normal, that doesn’t mean you need to suffer through them. If your symptoms feel overwhelming, know that there are treatment options to help reduce your discomfort.
Perimenopause: How to Take Control of Perimenopause Symptoms
For generations, we’ve done little to support or acknowledge women through this (often uncomfortable) transition. But, thankfully, more research is coming out about reproductive health. And, as a result, more insight into how to smooth out the more bumpy aspects of that journey.
This means you don’t need to grin and bear it as you struggle through heavy periods, overwhelming hot flashes, or painful intercourse. There are healthy habits and treatment options to help relieve some of your more concerning symptoms.5 Of course, please consult your healthcare provider before starting any treatment or making lifestyle changes.
Healthy Lifestyle Changes
Helps treat: most perimenopause symptoms
There are lifestyle changes you can implement that may help ease perimenopause, including:2 3 5
- Limiting caffeinated beverages and alcohol
- Avoiding hot flash triggers like hot environments, spicy foods, or hot beverages
- Enjoying a healthy diet with fruits, veggies, protein, healthy fats, and whole grains
- Adding a calcium supplement or multivitamin with calcium to your diet
- Exercising a few times a week (as recommended by the Physical Activity Guidelines for Americans)
- Wearing sweat-wicking or cooling clothing and plenty of layers to easily cool off
- Practicing meditation or other relaxation techniques
- Starting a relaxing nighttime routine so you can improve your sleep quality and quantity
- Quitting smoking
- Maintaining a healthy weight (as recommended by your doctor)
You may have also heard of herbal perimenopause supplements advertised to help lessen perimenopause symptoms. Keep in mind that supplements aren't regulated by the FDA. Talk to your doctor before you begin any new treatment option.2
Menopause Hormone Therapy
Helps treat: moderate to severe hot flashes, night sweats, heart palpitations, and vaginal dryness or discomfort
Menopause hormone therapy (also known as hormone replacement therapy) is a medication that is commonly understood to replace the hormones estrogen or estrogen and progesterone during perimenopause and menopause. This levels out your hormone fluctuations and, as a result, could help alleviate uncomfortable or painful symptoms like hot flashes, heart palpitations, and vaginal discomfort.6
And if you’ve had your ovaries removed (also known as surgical menopause) or stopped having periods before age 45 (also known as early menopause), estrogen therapy could also help decrease your risk of osteoporosis, heart disease, stroke, dementia, and mood shifts that might occur from less estrogen exposure over the years.6
As with all medical treatment, be sure to talk to your doctor about the best course of action given your personal medical history and the severity of your symptoms. Your doctor can help you weigh any potential risks given the type of hormone therapy used, the dosing, and how long you may be taking it.6 7
Antidepressants
Helps treat: mood swings, depression, and hot flashes
If you’re experiencing a large pendulum swing of emotions as a result of perimenopause, or other factors in your life, know that this is completely normal. Your risk of depression increases throughout perimenopause and menopause, especially if you have a history of PMDD or postpartum depression.8 Antidepressants could help regulate your mood. And research shows that low doses of antidepressants could also help tame hot flashes.3 9
Birth Control
Helps treat: mood swings, hot flashes, and heavy periods
Many women don’t realize that you can still get pregnant during perimenopause, even if your period is irregular. But taking birth control during this time can help with more than just preventing unwanted pregnancy. Low-dose birth control options like the pill, skin patch, vaginal ring, and progesterone injections could also help stabilize your mood, ease hot flashes, and reduce or eliminate a heavy flow.3 4 5
Vaginal Creams
Helps treat: vaginal dryness or discomfort
If you’re experiencing vaginal dryness or discomfort a vaginal cream could help. There are both over-the-counter and prescription options available that help restore vaginal moisture and acidity.5 And many can help make sexual intercourse a far more enjoyable experience. Make sure to talk to your doctor to learn about all available options and which one is best for you.6
When to See a Doctor
It’s a good idea to schedule time with your doctor as soon as you notice fluctuations in your period that might signal the start of perimenopause. Your doctor can help you understand if you’ve entered this transition by taking things like your menstrual cycle, symptoms, medical history, and age into account.2 12 They can also discuss and prescribe treatment options to make that transition smoother, especially if you’re experiencing symptoms like hot flashes or mood swings that are greatly affecting your quality of life.1 3
It’s also important to schedule regular check-ups with your doctor during this time because the decrease in estrogen during perimenopause can also lead to bone thinning and changing cholesterol levels.3 Your doctor can help ensure all things are proceeding smoothly, and, if necessary, suggest treatment options to keep you healthy.
Tracking Your Cycle
Even if you’re well acquainted with the menstrual cycle, it’s normal to feel in the dark about what’s going on in your body during perimenopause. But by tracking your cycle using a health device, you can shed a bit more light on what’s going on in your body — and help facilitate the conversation with your doctor.
With detailed symptom and mood tracking you can closely monitor every symptom, and notice trends you’re experiencing like changes in your mood, sleeping patterns, exercise performance, sex drive, and more. This data helps provide insight that could make your transition to menopause easier (or at least more understandable!).
The Takeaway
Perimenopause is your body’s natural transition to menopause. Although it’s often accompanied by new changes occurring in your body, know that there may be appropriate options for you to make this journey smoother. There are healthy lifestyle changes you can make like adjusting your sleeping habits and getting regular exercise. You can also stay informed and discover trends happening in your body by tracking your cycle and cycle-syncing your workouts. Plus there are treatment options available to you including hormone therapy, antidepressants, birth control, vaginal creams, and more. And don’t forget to schedule time with your doctor so they can assist you in this transition to your post-reproductive life.
Sources
- Perimenopause - Symptoms and causes. (2021, August 7). Mayo Clinic. Retrieved April 5, 2023, from https://www.mayoclinic.org/diseases-conditions/perimenopause/symptoms-causes/syc-20354666
- Perimenopause. (2021, August 8). Johns Hopkins Medicine. Retrieved April 5, 2023, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/perimenopause
- Perimenopause: Age, Stages, Signs, Symptoms & Treatment. (2021, October 5). Cleveland Clinic. Retrieved April 5, 2023, from https://my.clevelandclinic.org/health/diseases/21608-perimenopause
- Johnson, T. C. (2022, July 1). Perimenopause. WebMD. Retrieved April 5, 2023, from https://www.webmd.com/menopause/guide/guide-perimenopause
- Perimenopause: Rocky road to menopause. (2022, August 9). Harvard Health. Retrieved April 5, 2023, from https://www.health.harvard.edu/womens-health/perimenopause-rocky-road-to-menopause
- Hormone therapy: Is it right for you? (2022, December 6). Mayo Clinic. Retrieved April 5, 2023, from https://www.mayoclinic.org/diseases-conditions/menopause/in-depth/hormone-therapy/art-20046372
- Hormone Therapy for Menopause: Types, Benefits & Risks. (2021, June 28). Cleveland Clinic. Retrieved April 5, 2023, from https://my.clevelandclinic.org/health/treatments/15245-hormone-therapy-for-menopause-symptoms
- Parry, B. L. (2010). Optimal management of perimenopausal depression. International Journal of Women’s Health, 143. https://doi.org/10.2147/ijwh.s7155
- Wu, C., Tseng, P., Wu, M., Li, D., Chen, T., Kuo, F., Stubbs, B., Carvalho, A. F., Chen, Y., Lin, P., Cheng, Y., & Sun, C. (2020). Antidepressants during and after Menopausal Transition: A Systematic Review and Meta-Analysis. Scientific Reports, 10(1). https://doi.org/10.1038/s41598-020-64910-8
- Can You Take Antidepressants for Menopause Symptoms? How SSRIs May Reduce Hot Flashes. (2022, June 28). GoodRx Health. Retrieved April 5, 2023, from https://www.goodrx.com/conditions/menopause/antidepressants-for-menopause
- Postmenopause: Signs, Symptoms & What to Expect. (2021, October 5). Cleveland Clinic. Retrieved April 17, 2023, from https://my.clevelandclinic.org/health/diseases/21837-postmenopause
- Perimenopause - Diagnosis and treatment. (2021, August 7). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/perimenopause/diagnosis-treatment/drc-20354671